Hamstring Injuries
Hamstring Injuries: High energy and extension issues
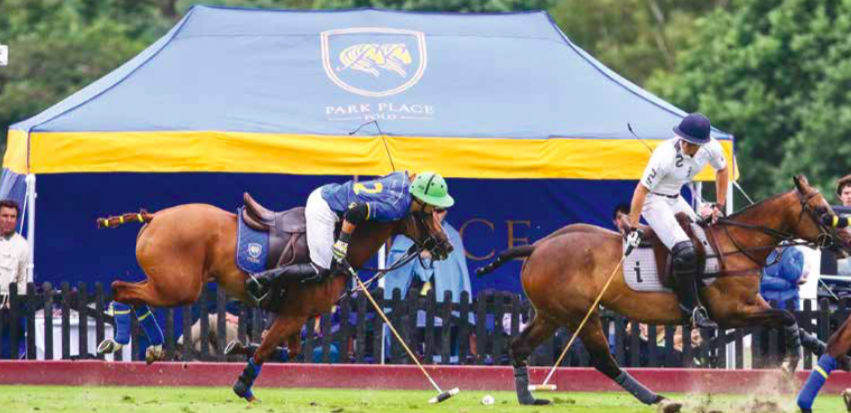
A powerful eccentric contraction can injure the hamstring tendon when extending too far out of the saddle
(Dr. med. Andreas Krüger @polotimes.co.uk)
The hamstring comprises most of the muscle bulk in the back of the thigh. It is important for pushing off, jumping and landing and particularly when riding for ensuring good contact to the saddle. The hamstring is made up of three muscles – the biceps femoris, the semitendinosus and the semimembranosus, each with a common proximal attachment via a large tendon to the ischial tuberosity of the pelvis (the large bone you sits on in the buttock). This proximal attachment provides a fixed point from which muscle contraction can affect a more distal action – the hamstring provides some hip extension, but the main action is movement around the knee. This is the main muscle group responsible for knee flexion. The sciatic nerve runs very close to the proximal tendon attachment to the ischium and can be injured together with the hamstring.
Mechanism of injury
Powerful eccentric contraction, i.e. not placed centrally, either injures the proximal hamstring tendon through a progressive stretch or more commonly, when the hip is suddenly and forcefully flexed over an extended knee. This happens when you try to stay in the saddle while falling and the horse adds an additional opposite force. Proximal hamstring injuries can be complete tendon ruptures or incomplete/ partial tears. In a young person, the bone with the tendon attached is often separated or fractured from the pelvis (ischium).
Presentation of a hamstring injury
The rider will feel something ‘go’, deep in the buttock. If the incident is observed by others, often the player will grab the buttock or upper thigh – the so called ‘clutch’ sign of a hamstring injury. They are generally not able to continue with activity and if on the ground may need assistance to get up and walk. There is usually immediate pain and weight bearing on the affected leg is very difficult, so crutches are usually required. It is painful to sit on the affected buttock. Over the next 24 to 48 hours there is usually swelling and bruising that appears over the buttock area, which then extends down the back of the thigh and sometimes even into the lower leg. Occasionally there can be pins and needles in the foot or lower leg and loss of movement in the foot can be seen with a foot drop in rare cases.
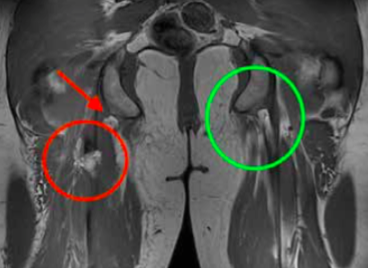
An MRI is the gold standard for identifying hamstring tendon tears. The red circle signifies an injured tendon, whereas the green circle shows a healthy tendon.
Investigation: X-rays
X-rays are important for younger patients, to rule out a fracture of the bony attachment.
Ultrasound
Ultrasound can identify a blood collection in the buttock and upper thigh, whilst also detecting tendon tears.
MRI
An MRI scan is the gold standard which is highly accurate at determining the site of injury, whether the tear is partial or complete and importantly whether there has been any retraction of the tendon end into the thigh.
A powerful eccentric contraction can injure the hamstring tendon when extending too far out of the saddle (Photography by imagesofpolo.com)
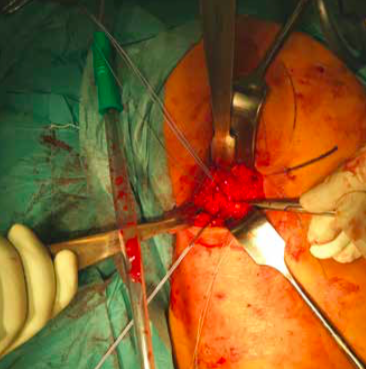
Operative repair of a hamstring tendon is recommended when there is a complete tear
The incision is made in the buttock/upper thigh area where the torn tendon end will be found
Treatment
Initial treatment in the first few days should be symptomatic – measures to reduce pain and swelling with icing, analgesia and the use of crutches to assist walking. As the pain starts to settle, some gentle movement of the leg can be beneficial and the assistance of a physiotherapist at this point can be very helpful.
Once the diagnosis of a hamstring injury is made, it is important to get a specialist opinion regarding treatment options. Conservative treatment with a rehab programme may be appropriate for players with a low demand, or those with partial tendon tears where a significant proportion of the tendon is still intact. Operative repair of the tendon is generally recommended when there is a complete tendon tear. Surgical repair usually involves an overnight stay in hospital and the procedure itself is performed under general anaesthetic. An incision is made in the buttock/upper thigh and the torn tendon end is identified, mobilised if it is retracted down into the thigh and then repaired back onto the bone using bone anchor sutures.
Rehabilitation
After surgery, painkillers are generally required. Post-operation, a positioning pillow under the knees will relax the hamstring and a leg brace will control the degree of extension. Initially the knee will be limited to a 60 degree flexion. A systematic progression of extension is advised in two-week intervals, increasing the extension in 20 degree steps. Crutches will be needed for six weeks, putting a small amount of weight on the ground and the extension of the knee is limited with a brace. At six weeks, patients will start loading of the leg with possibly a return to light running and soft riding at three to four months. A return to chukkas may be considered after six months.
Physiotherapy protocol
(by Gregor Schwarzer, Gsports.ch)
It is important to know how the region of the lower back/pelvis/ hip is put together. The physiotherapy programme following surgery will be divided in four periods of time:
Period One
Day 0 to 5: Vascular and cellular phase with inflammation control. This is the healing phase of the skin and the soft tissue underneath. It is essential to control inflammation of the vascular and cellular phase.
Period Two
Day 5 to 20: Proliferation. The healing from Period One will continue whilst a scar is created on the surface.
Period Three
Day 21 to 60: Consolidation of work. The wound’s scar tissue should be stable by this point, so the rehabilitation is now about consolidation.
Period Four
Day 60 and onwards: Organisation and reconstruction (the most important element).
The adequate stimulus of the tendon matrix is the most crucial element when finding the way back to full function, following a strict regime according to the aforementioned periods.
Rehabilitation
Day 1 to 21: Local therapy is required. Start with lumbar spine treatment as well as treatment to the hip/leg region. Day 21 to 42: Testing the trunk musculature and control of the body’s symmetries. Day 42 onwards: Begin your return to activity while undertaking quality exercises. To regain your former activity level will be challenging.
For more information contact Dr. med. Andreas Krüger
Dr.med. Andreas Krüger is a Swiss board orthopaedic and trauma surgeon in Zurich, who specialises in knee and shoulder surgery. Andi is a second generation of tournament doctors for equine sports, known as Polodoc since 2013 and is a member at Legacy Polo Club in Switzerland