DR. MED. ANDREAS KRÜGER (MD, POLODOC)
Specialist in Orthopaedic Surgery and Traumatology FMH
Hamstring Injuries
The hamstring comprises most of the muscle bulk in the back of the thigh. It is important for pushing off, jumping and landing and particularly when riding for ensuring good contact to the saddle. The hamstring is made up of three muscles – the biceps femoris, the semitendinosus and the semimembranosus, each with a common proximal attachment via a large tendon to the ischial tuberosity of the pelvis (the large bone you sits on in the buttock).
Hamstring Injuries: High energy and extension issues
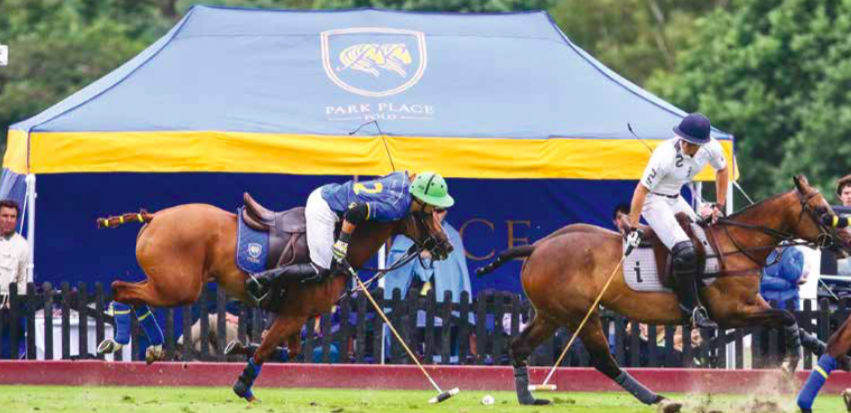
A powerful eccentric contraction can injure the hamstring tendon when extending too far out of the saddle
(Dr. med. Andreas Krüger @polotimes.co.uk)
The hamstring comprises most of the muscle bulk in the back of the thigh. It is important for pushing off, jumping and landing and particularly when riding for ensuring good contact to the saddle. The hamstring is made up of three muscles – the biceps femoris, the semitendinosus and the semimembranosus, each with a common proximal attachment via a large tendon to the ischial tuberosity of the pelvis (the large bone you sits on in the buttock). This proximal attachment provides a fixed point from which muscle contraction can affect a more distal action – the hamstring provides some hip extension, but the main action is movement around the knee. This is the main muscle group responsible for knee flexion. The sciatic nerve runs very close to the proximal tendon attachment to the ischium and can be injured together with the hamstring.
Mechanism of injury
Powerful eccentric contraction, i.e. not placed centrally, either injures the proximal hamstring tendon through a progressive stretch or more commonly, when the hip is suddenly and forcefully flexed over an extended knee. This happens when you try to stay in the saddle while falling and the horse adds an additional opposite force. Proximal hamstring injuries can be complete tendon ruptures or incomplete/ partial tears. In a young person, the bone with the tendon attached is often separated or fractured from the pelvis (ischium).
Presentation of a hamstring injury
The rider will feel something ‘go’, deep in the buttock. If the incident is observed by others, often the player will grab the buttock or upper thigh – the so called ‘clutch’ sign of a hamstring injury. They are generally not able to continue with activity and if on the ground may need assistance to get up and walk. There is usually immediate pain and weight bearing on the affected leg is very difficult, so crutches are usually required. It is painful to sit on the affected buttock. Over the next 24 to 48 hours there is usually swelling and bruising that appears over the buttock area, which then extends down the back of the thigh and sometimes even into the lower leg. Occasionally there can be pins and needles in the foot or lower leg and loss of movement in the foot can be seen with a foot drop in rare cases.
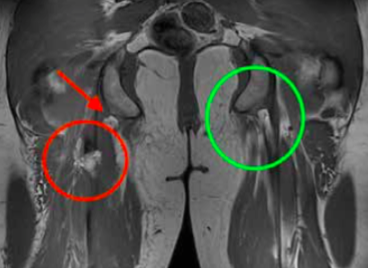
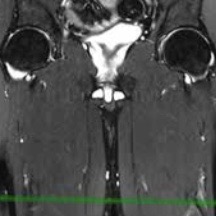
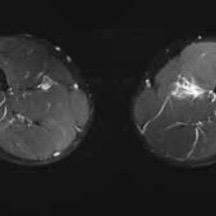
An MRI is the gold standard for identifying hamstring tendon tears. The red circle signifies an injured tendon, whereas the green circle shows a healthy tendon.
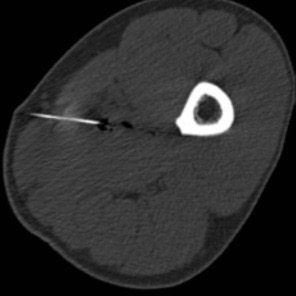
Investigation: X-rays
X-rays are important for younger patients, to rule out a fracture of the bony attachment.
Ultrasound
Ultrasound can identify a blood collection in the buttock and upper thigh, whilst also detecting tendon tears.
MRI
An MRI scan is the gold standard which is highly accurate at determining the site of injury, whether the tear is partial or complete and importantly whether there has been any retraction of the tendon end into the thigh.
A powerful eccentric contraction can injure the hamstring tendon when extending too far out of the saddle (Photography by imagesofpolo.com)
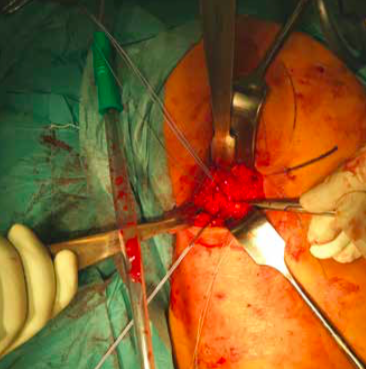
Operative repair of a hamstring tendon is recommended when there is a complete tear
The incision is made in the buttock/upper thigh area where the torn tendon end will be found
Treatment
Initial treatment in the first few days should be symptomatic – measures to reduce pain and swelling with icing, analgesia and the use of crutches to assist walking. As the pain starts to settle, some gentle movement of the leg can be beneficial and the assistance of a physiotherapist at this point can be very helpful.
Once the diagnosis of a hamstring injury is made, it is important to get a specialist opinion regarding treatment options. Conservative treatment with a rehab programme may be appropriate for players with a low demand, or those with partial tendon tears where a significant proportion of the tendon is still intact. Operative repair of the tendon is generally recommended when there is a complete tendon tear. Surgical repair usually involves an overnight stay in hospital and the procedure itself is performed under general anaesthetic. An incision is made in the buttock/upper thigh and the torn tendon end is identified, mobilised if it is retracted down into the thigh and then repaired back onto the bone using bone anchor sutures.
Rehabilitation
After surgery, painkillers are generally required. Post-operation, a positioning pillow under the knees will relax the hamstring and a leg brace will control the degree of extension. Initially the knee will be limited to a 60 degree flexion. A systematic progression of extension is advised in two-week intervals, increasing the extension in 20 degree steps. Crutches will be needed for six weeks, putting a small amount of weight on the ground and the extension of the knee is limited with a brace. At six weeks, patients will start loading of the leg with possibly a return to light running and soft riding at three to four months. A return to chukkas may be considered after six months.
Physiotherapy protocol
(by Gregor Schwarzer, Gsports.ch)
It is important to know how the region of the lower back/pelvis/ hip is put together. The physiotherapy programme following surgery will be divided in four periods of time:
Period One
Day 0 to 5: Vascular and cellular phase with inflammation control. This is the healing phase of the skin and the soft tissue underneath. It is essential to control inflammation of the vascular and cellular phase.
Period Two
Day 5 to 20: Proliferation. The healing from Period One will continue whilst a scar is created on the surface.
Period Three
Day 21 to 60: Consolidation of work. The wound’s scar tissue should be stable by this point, so the rehabilitation is now about consolidation.
Period Four
Day 60 and onwards: Organisation and reconstruction (the most important element).
The adequate stimulus of the tendon matrix is the most crucial element when finding the way back to full function, following a strict regime according to the aforementioned periods.
Rehabilitation
Day 1 to 21: Local therapy is required. Start with lumbar spine treatment as well as treatment to the hip/leg region. Day 21 to 42: Testing the trunk musculature and control of the body’s symmetries. Day 42 onwards: Begin your return to activity while undertaking quality exercises. To regain your former activity level will be challenging.
For more information contact Dr. med. Andreas Krüger
Dr.med. Andreas Krüger is a Swiss board orthopaedic and trauma surgeon in Zurich, who specialises in knee and shoulder surgery. Andi is a second generation of tournament doctors for equine sports, known as Polodoc since 2013 and is a member at Legacy Polo Club in Switzerland
Protect Your Muscles
The most common cause of groin pain is a muscle, tendon or ligament strain, particularly in athletes who play stop and go sports. Groin pain might occur immediately after an injury, or pain may come on gradually over a period of weeks or even months and will be worsened by continued use of the injured area. Less commonly, a bone injury or fracture, a hernia or even kidney stones might cause groin pain. Although testicle pain and groin pain are different, a testicle condition can sometimes cause pain that spreads to the groin area.
Tune up the brakes – Optimise the muscle
(Dr. med. Andreas Krüger @polotimes.co.uk) Polodoc Medical Insight September 2017
Stopping the horse and keeping the position in the saddle while changing direction can create extreme tension to the thigh musculature. This peak tension can damage a cold or not prepared muscle. A strain, muscle pull, or even a muscle tear refers to damage to a muscle or its attaching tendons. You can put undue pressure on muscles during normal riding, normal daily activities, with sudden heavy lifting, during sports, or while performing work tasks.
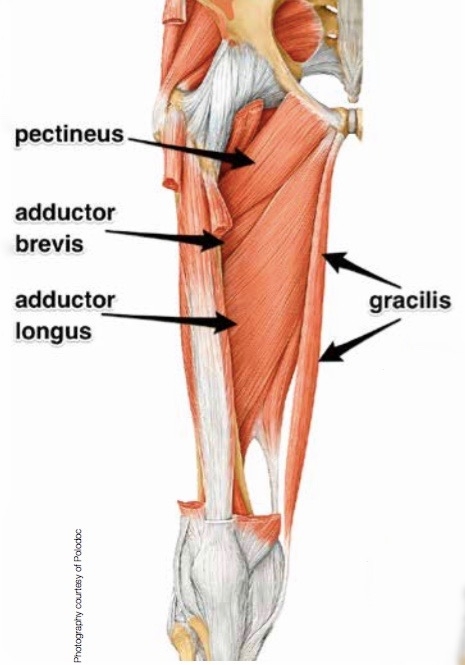
Injury pattern
Muscle damage can be in the form of tearing (part or all) of the muscle bres and the tendons attached to the muscle. The tearing of the muscle can also damage small blood vessels, causing local bleeding, or bruising and pain caused by irritation of the nerve endings in the area. Typical injury happens when the player is not warmed up and pre-riding stretching was left out, in particular, the half seat and braking, needs maximum contraction of the adductor muscles.
Symptoms of muscle strain
Swelling, bruising, or redness due to the injury
Pain at rest
Pain when the speci c muscle or the joint in relation to that muscle is used
Weakness of the muscle or tendons
Inability to use the muscle at all
Diagnosis
In most of the cases, the injury history, the injury pattern and clinical examination help to de ne the diagnosis.
First line treatment
The muscle pattern of the upper thigh and adductor
Protect the strained muscle from further injury and rest the strained muscle. Avoid the activities which caused the strain and other painful activities. Ice the muscle area (20 minutes every hour while awake). Ice is a very effective anti-in ammatory and pain- reliever. Small ice packs, such as packages of frozen vegetables or water frozen in foam coffee cups, applied to the area may help decrease in ammation. Compression can be gently applied with an Ace or other elastic bandage, which can both provide support and decrease swelling. Do not wrap tightly and elevate the injured area to decrease swelling, propping up a strained leg muscle while sitting, for example. Activities that increase muscle pain or work the affected body part are not recommended until the pain has signi cantly improved.
Professional treatment
The most important key to treatment is the early diagnostic proof of a working diagnosis from clinical examination. Ultrasound is the best form of examination where the exact point of maximum pain can be detected, while the MRI (Magnetic Resonance Imaging) is most precise in de ning the extent of injury in a standardised fashion. Following this a computer tomography guided in ltration can deliver painkillers (Ketorolac) directly to the spot of the lesion with additional PRP (Platet-riched Plasma - ACP or Hyaloron Tendon) for accelerated healing. After treatment, physical workouts should be limited the frst 48 hours. A physiotherapeutic workout should consist of an eccentric training with local analgesic treatment (Ultrasound, TENS). The new Compex® SP 8.0 treatment programmes can alleviate pain, measuring the individual impulse needed to optimally stimulate the muscle. At the same time, muscle training should also be undertaken. Beyond this manual treatment, auxiliary local compression with thigh sleeves may also reduce the symptoms.
An MRI Scan can be the most useful diagnostic tool
When adequate stretching has not taken place before ..
... a match, injuries to the muscles becomes more likely
Return to play
The intervals between injury and a return to sport are different for each individual. After a minimum of three weeks recovery, pain free normal gait and a less than few seconds squeeze test are mandatory perquisites to go back in the saddle. In the worst cases of muscle injury, even longer periods are recommended.
Electrical stimulation can also help speed up recovery
Prevention
Most muscle injuries are due to a neglected preparation timetable for the maximum load and strain on the tissue. Also, repetitive micro injuries can lead to chronic impairment. Elasticity of the muscle is key, so adequate stretching before and after the game is crucial. Optimal preparation with additional workout through electrical stimulation may also be helpful.
Stretching before and after the match is important to prevent injury
When to see your doctor
Hematoma in the region of pain
Palpable cavity in the muscle
Ongoing pain for more than one week
Rule out symphysis injury
For more information contact Dr. med. Andreas Krüger